Health Plan Administration
Claims Adjudication
SIHO's Claims Department receives extensive claims processing training that includes knowledge on ICD-10, CPT procedure codes, diagnosis codes, medical terminology, as well as fraud and abuse procedures. Each year, the Claims department processes over 2 million medical and dental claims.
Claims are received electronically as well as on paper. Currently, approximately 85% of all claims are received electronically. The average turnaround time from receipt to processed date for all claims is 4-6 days. The claims department strives to keep no more than 5 days’ work on hand at any time in order to maintain timeliness.
Claims Auditing
Claims Analysts are audited at 100% during the training period as well as during the learning period following training. After training is complete, regular audits are done on a monthly and quarterly basis to ensure both financial and benefit accuracy.
In addition to auditing the Claim Analyst, when a group switches to SIHO or at the time of benefit changes, extensive auditing occurs to ensure accuracy in the system set-up before any claims are adjudicated.
About Member Services
SIHO's staff of highly trained Member Service Representatives are available to help answer any questions pertaining to the health plans SIHO administers. Inquiries include benefit coverage questions, claim inquiries, and providers verifying coverage and benefits. Member Service Representatives are required to log all calls on SIHO’s integrated system. Calls are also routinely monitored by management personnel to ensure SIHO is providing quality service to our clients.
Integrated Call Center Technology
SIHO's state-of-the-art telephone system has comprehensive monitoring and audit capability to ensure SIHO continuously monitors its service levels to meet the needs of each caller. Our automated call distribution system is a combination of specifically designed hardware and software that has been engineered to be the most flexible integrated technology available in the industry to further enhance member satisfaction.
Walk-in Availability
One of the unique features of SIHO’s Member Services is the option for members to come in and meet with our Member Service Representatives face-to-face in our corporate headquarters office in Columbus, IN. Whether a member would like to walk-in and pick up forms or discuss the intricacies of a complex benefit situation, members are always welcome. If a member would like to meet outside of normal business hours, arrangements can be made for after-hours appointments.
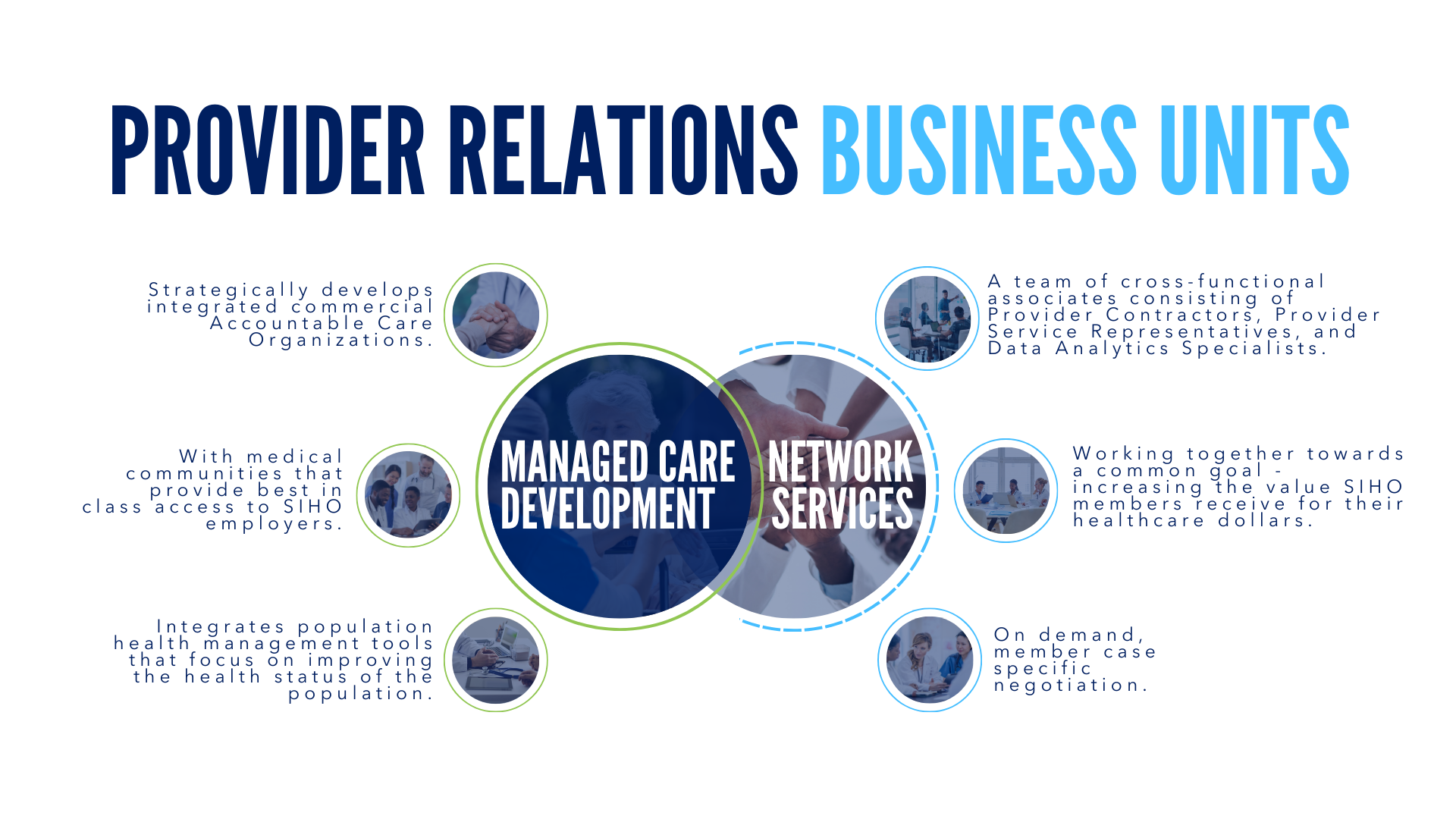
Network Services
SIHO’s Provider Relations department develops strong relationships with medical communities, adding both financial and qualitative benefits to SIHO members. Our dedicated team of professionals focuses on cost containment initiatives, allowing employers access to networks and products that reduce healthcare costs and improve quality.
SIHO has developed a comprehensive solution for provider networks that offers members regional and national access through our proprietary and Preferred Provider Organization (PPO) network partners.
Medical Management
SIHO’s Medical Management offers a wide range of quality health programs. Our staff consists of highly qualified Physicians and Registered Nurses whose primary goal is to ensure that our members receive the clinically necessary and appropriate care in the right setting; the care is cost-effective; and the care results in improved functional, financial and clinical outcomes.
Another feature of our Medical Management Program is that the program is locally managed. This enables us to have a better understanding of the needs of the members, employers, and physicians. SIHO streamlines administrative procedures, enabling us to concentrate more on our members’ health.
At the very core of the Medical Management Program is our claims and pharmacy data. This data is analyzed to determine if interventions are required. The findings are shared with providers, members, and employers on a group level. SIHO provides information to members and providers, allowing them to make the best health care choices for both the patient and the practice. SIHO implements successful interventions by monitoring and measuring data to assure improved outcomes.
Our Medical Management team consists of the following personnel located across several geographic markets.
- 5 Part-Time Medical Directors
- Certified Case Managers
- Nurses Certified and specializing in the following areas
- Oncology
- Cardiovascular Certified Advanced Practice
- Mental Health
- Transplant Coordinator
- Hospice
- Emergency Medicine
Population Health
SIHO provides a continuum of three tools to manage the utilization of healthcare resources. These range from a foundation of Core Medical Management Services up to the most comprehensive program of Population Management. As an employer progresses through this continuum, often through a multi-year migration, the intensity of services increase as illustrated below:


Wellness
At SIHO we understand how challenging it can be to find the time to design and implement an effective wellness program. Balancing the health and productivity of your employees amidst other priorities can be hectic, but our optional Wellness Works program can help you and your employees reach that sense of harmony. Employers can choose from any three of our wellness plan designs to suit their needs. Our Wellness Works team will work with your business to bring a complete solution to the table.
Some of the services our Wellness Works program offers are:

